Abstract
Attention biases towards threatening and sad stimuli are associated with pediatric anxiety and depression, respectively. The basic cognitive mechanisms associated with attention biases in youth, however, remain unclear. Here, we tested the hypothesis that threat bias (selective attention for threatening versus neutral stimuli) but not sad bias relies on stimulus-driven attention. We collected measures of stimulus-driven attention, threat bias, sad bias, and current clinical symptoms in youth with a history of an anxiety disorder and/or depression (ANX/DEP; n=40) as well as healthy controls (HC; n=33). Stimulus-driven attention was measured with a non-emotional spatial orienting task, while threat bias and sad bias were measured at a short time interval (150 ms) with a spatial orienting task using emotional faces and at a longer time interval (500 ms) using a dot-probe task. In ANX/DEP but not HC, early attention bias towards threat was negatively correlated with later attention bias to threat, suggesting that early threat vigilance was associated with later threat avoidance. Across all subjects, stimulus-driven orienting was not correlated with early threat bias but was negatively correlated with later threat bias, indicating that rapid stimulus-driven orienting is linked to later threat avoidance. No parallel relationships were detected for sad bias. Current symptoms of depression but not anxiety were related to decreased stimulus-driven attention. Together, these results are consistent with the hypothesis that threat bias but not sad bias relies on stimulus-driven attention. These results inform the design of attention bias modification programs that aim to reverse threat biases and reduce symptoms associated with pediatric anxiety and depression.
Keywords: Anxiety, Depression, Threat Bias, Sad Bias, Attention Bias, Stimulus-driven Attention, Adolescent
Anxiety disorders and depression are common, debilitating mental health disorders with symptoms that often emerge during childhood (Merikangas et al., 2010). Emerging evidence suggests that selective attention to negative stimuli is related to the etiology of anxiety and depression in both youth (Eldar, Ricon, & Bar-Haim, 2008) and adults (MacLeod, Rutherford, Campbell, Ebsworthy, & Holker, 2002). In adults, anxiety has been robustly associated with attention bias to threatening stimuli (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & van IJzendoorn, 2007), while depression has been linked with attention bias to sad stimuli (Peckham, McHugh, & Otto, 2010). Although attention biases to negative stimuli have also been associated with pediatric anxiety and depression, the patterns of attention biases in youth are less clear compared to adults (Pine, Helfinstein, Bar-Haim, Nelson, & Fox, 2009; Puliafico & Kendall, 2006; Shechner et al., 2012). This lack of clarity represents an important gap in the literature in understanding how attention biases develop and become stable. Despite the incomplete characterization of attention biases in youth, computer-based programs have been shown to reduce attention biases to negative stimuli and alleviate symptoms of anxiety and depression in adolescents (Eldar et al., 2012; Lowther & Newman, 2014; Shechner et al., 2014) as well as adults (Browning, Holmes, Charles, Cowen, & Harmer, 2012; Hakamata et al., 2010). Given that anxiety and depression in childhood and adolescence may represent the onset of an aberrant neurodevelopmental cascade (Pine, 2007), coupled with the observation that childhood is a period of relatively greater neuroplasticity, elucidating and modifying attention biases in children may represent a unique opportunity to prevent a lifetime of symptoms. Unfortunately, the basic cognitive and neurobiological mechanisms associated with attention biases, especially in youth, remain poorly understood.
Work in adults suggests that the maladaptive pattern of attention to threat associated with anxiety disorders differs from the pattern of attention to sad stimuli associated with depression. Anxiety symptoms and disorders in adults are associated with a vigilance-avoidance pattern of attention to threatening stimuli (Cisler & Koster, 2010; Mogg, Bradley, Miles, & Dixon, 2004). Immediately after a threatening stimulus appears, highly anxious individuals orient more rapidly (Koster, Crombez, Verschuere, Van Damme, & Wiersema, 2006; Mogg, Bradley, de Bono, & Painter, 1997) and have greater difficulty disengaging attention from the threatening stimulus (Amir, Elias, Klumpp, & Przeworski, 2003; Fox, Russo, Bowles, & Dutton, 2001; Koster, Verschuere, Crombez, & Van Damme, 2005) relative to low-anxious individuals. At longer durations, however, adults with high anxiety attend away from or avoid threatening stimuli (Koster, Baert, Bockstaele, & De Raedt, 2010; Koster et al., 2005; Mogg et al., 2004). Depressive symptoms and disorders, in contrast, have been robustly linked to difficulty disengaging attention from sad stimuli even at longer durations (Bradley, Mogg, & Lee, 1997; Sanchez, Vazquez, Marker, LeMoult, & Joormann, 2013; Teachman, Joormann, Steinman, & Gotlib, 2012). Most evidence indicates that depressed adults do not, however, orient more rapidly to sad stimuli compared to non-depressed individuals (Cisler & Koster, 2010; Teachman et al., 2012), but depressed adults tend to linger attention on sad stimuli for several seconds after stimulus onset (Peckham et al., 2010).
The patterns of attention biases in anxious and depressed youth to threatening and sad stimuli are less clear. Although there is also experimental evidence for a vigilance-avoidance pattern of attention to threatening stimuli in anxious youth (In-Albon, Kossowsky, & Schneider, 2010), the pediatric literature is mixed with many reports of threat vigilance in anxiety (Dalgleish et al., 2003; Roy et al., 2008; Taghavi, Neshat-Doost, Moradi, Yule, & Dalgleish, 1999; Vasey, Daleiden, Williams, & Brown, 1995; Waters, Henry, Mogg, Bradley, & Pine, 2010; Waters, Mogg, Bradley, & Pine, 2008), but also several reports of threat avoidance (Britton et al., 2012; Brown et al., 2013; Monk et al., 2006). More work is needed to determine whether the mixed pediatric literature is partly a result of threat vigilance in studies that measure threat bias at short durations and threat avoidance in studies that measure threat bias at long durations. Two studies examining eye movements to emotional faces have reported early threat vigilance in anxious youth but failed to detect later threat avoidance (Seefeldt, Kramer, Tuschen-Caffier, & Heinrichs, 2014; Shechner et al., 2013). The reasons for the mixed literature in youth are multifactorial and may include developmental considerations, sample selection, and task design (Pine et al., 2009; Puliafico & Kendall, 2006; Shechner et al., 2012). Studies of sad bias associated with depression in youth are relatively rare, with both attention bias towards sad stimuli (Hankin, Gibb, Abela, & Flory, 2010) and attention bias away from sad stimuli (Harrison & Gibb, 2014) reported. Youth with comorbid anxiety and depression appear to exhibit attention bias towards both threatening and sad stimuli (Harrison & Gibb, 2014). Further studies are warranted that describe the pattern of attention biases in anxious and depressed youth.
In addition to these associations with active symptoms, attention biases appear to confer risk for the development of anxiety and depression. School-age daughters of depressed mothers, at high risk for depression on the basis of family history, exhibit an attention bias towards (Joormann, Talbot, & Gotlib, 2007; Kujawa et al., 2011) or away (Gibb, Benas, Grassia, & McGeary, 2009) from sad stimuli, while daughters of mothers with panic disorder exhibit a bias towards physical health-related threat cues (Mogg, Wilson, Hayward, Cunning, & Bradley, 2012). Infants and toddlers with high behavioral inhibition, a temperamental risk factor for anxiety and depression (Fox, Henderson, Marshall, Nichols, & Ghera, 2005), develop social withdrawal as young children (Perez-Edgar et al., 2011) and adolescents (Pérez-Edgar et al., 2010) only if they also exhibit an attention bias towards threat. Because attention acts as a filter to further processing, children with attention biases towards negative stimuli may have a disproportionately more intense experience with negative stimuli (Derryberry & Reed, 2002; Derryberry & Rothbart, 1997; Lonigan, Vasey, Phillips, & Hazen, 2004), conferring risk for anxiety and depression. As such, it is especially important to study mechanisms underlying threat and sad biases in children, because attention biases may be the gateway to an aberrant neurodevelopmental cascade resulting in symptoms of depression and anxiety in adulthood (Pine, 2007).
The vigilance-avoidance pattern of attention to threatening stimuli in anxiety versus the difficulty disengaging from sad stimuli in depression suggests that different basic attention processes are involved, even though the same individual may exhibit both biases. One hypothesis is that anxiety symptoms are associated with automatic orientation of attention to threatening stimuli whereas depressive symptoms are associated with non-automatic, goal-directed attention to sad stimuli (Cisler & Koster, 2010; Teachman et al., 2012; Williams, Watts, MacLeod, & Mathews, 1997). This distinction parallels the division between ‘stimulus-driven’ and ‘goal-directed’ attention in a common biologically informed model of spatial attention (Chica, Bartolomeo, & Lupianez, 2013; Corbetta & Shulman, 2002). In this model, stimulus-driven attention refers to the involuntary orientation of attention to the location of salient stimuli shortly after they appear (< 150ms). This rapid orientation of attention towards salient stimuli is followed by a shift away from the location of the stimulus within 500ms, a phenomenon referred to as inhibition of return (Klein, 2000). Early automatic orientation followed by later inhibition of return may parallel the vigilance and avoidance phases of attention to threat in anxiety, although some evidence suggests that the avoidance phase is a goal-directed, adaptive process that serves to minimize distress (Derryberry & Reed, 2002; Lonigan & Vasey, 2009; Lonigan et al., 2004). In contrast to stimulus-driven attention, goal-directed attention refers to the slower (~500ms), voluntary shift of attention to locations based on an individual's current goals and is generally not associated with inhibition of return. Sad bias in depression unfolds over time in a manner consistent with goal-directed attention.
A limited evidence base suggests that attention mechanisms themselves, irrespective of emotional content, may be altered in youth with anxiety and/or depression. According to Eysenck's attentional control theory, anxiety disorders are associated with increased stimulus-driven attention and decreased goal-directed attention, regardless of emotional content of stimuli (Eysenck, Derakshan, Santos, & Calvo, 2007). Consistent with this theory, a study of adults reported faster stimulus-driven attention to non-emotional stimuli in participants with high trait anxiety relative to adults with low trait anxiety (Pacheco-Unguetti, Acosta, Callejas, & Lupiáñez, 2010). Furthermore, studies in both youth (Hogan, Butterfield, Phillips, & Hadwin, 2007) and adults (Bruder et al., 2002; Li, Hu, Liu, & Wu, 2011) support an increase in specific electroencephalographic (EEG) signals that may reflect stimulus-driven attention associated with symptoms of anxiety. Interestingly, a few studies suggest that these same EEG signals, possibly reflecting stimulus-driven attention, are decreased in depression (Bruder et al., 2002; Li et al., 2011; lv, Zhao, Gong, Chen, & Miao, 2010), and it has been proposed that depression is associated with decrements in both stimulus-driven and goal-oriented attention (Sylvester et al., 2012).
The evidence reviewed above suggests that attention biases are important keys to the developmental psychopathology and, potentially, to the treatment of youth with anxiety disorders and depression. Elucidating mechanisms of attention bias in youth may inform the design of treatments to modify these biases earlier in life and potentially prevent a cascade of pathology. In the present study, we explored three related issues. First, we tested the hypothesis that the magnitude of threat bias but not sad bias is associated with stimulus-driven attention. We predicted that an individual's stimulus-driven attention to generic, non-emotional stimuli should be related to that individual's attention bias towards threatening but not sad stimuli. Second, we explored the relationship between current symptoms of anxiety and depression and stimulus-driven attention. As above, limited data suggest that stimulus-driven attention is positively associated with symptoms of anxiety but negatively correlated with symptoms of depression. Finally, we examined whether the relationship between stimulus-driven attention and threat bias varies depending on clinical history. Stimulus-driven attention may be linked to attention bias towards threat but not sad stimuli in all children or exclusively in children with a history of anxiety or depression.
To address these issues, we collected measures of stimulus-driven attention, threat bias, sad bias, and current clinical symptoms of anxiety and depression in a well-characterized longitudinal cohort of youth with a history of an anxiety disorder and/or depression (preschool onset depression or DSM-IV-TR defined major depressive disorder) as well as healthy controls with no psychiatric history (Luby, Si, Belden, Tandon, & Spitznagel, 2009). Previous work in this sample demonstrated a significant relationship between attention bias toward threat and resting state functional connectivity of the ventral attention network, a functional brain network putatively involved in stimulus-driven attention (Sylvester et al., 2013). This earlier study provides some initial, indirect evidence that stimulus-driven attention may be related to attention bias towards threat. Diagnostic data are available in annual waves in this cohort from age three to six years through the time of the current study (average age 12.9 years). We took advantage of the high comorbidity between anxiety disorders and depression in the study sample to investigate threat bias and sad bias in the same cohort in order to minimize uncontrolled group differences as a confounding factor. Given that many of the youth in this study had a history of an anxiety disorder or depression, this sample represents a critical target population to inform the design of treatments that modify attention biases.
METHOD
Participants
The Institutional Review Board at Washington University School of Medicine approved all procedures. Subjects were drawn from the ongoing Validation of Preschool Depression Study for which detailed methods have been previously described (Luby, Belden, Pautsch, Si, & Spitznagel, 2009; Luby, Si, et al., 2009). As an overview, beginning in 2002, children aged three to six years were screened from primary care sites and oversampled for symptoms of depression; psychiatric and healthy control subjects were also obtained. This rich dataset includes longitudinal sociodemographic, clinical, and neuroimaging measures. A subset of subjects with a history of an anxiety disorder and/or depression as well as healthy controls was invited to participate in a variety of attention tasks for the current study.
We divided subjects into youth with a history of an anxiety disorder and/or depression (ANX/DEP) and healthy controls (HC). Anxiety disorders included separation anxiety disorder, generalized anxiety disorder, social phobia, agoraphobia, and specific phobia. HC children had no history of any psychiatric disorder. Annual diagnostic assessments were determined by parent report on the Preschool-Age Psychiatric Assessment (Egger, Ascher, & Angold, 2003) for children aged 8.0 years and younger and by combined parent and child report (from separate interviews) (Bird, Gould, & Staghezza, 1992) on the Child and Adolescent Psychiatric Assessment (Angold & Costello, 2000) for children older than 8.0 years. Trained staff conducted interviews and established procedures maintained inter-rater reliability. The duration criterion was set aside for a diagnosis of depression arising during the preschool period (before age six) (Gaffrey, Belden, & Luby, 2011). Group status was based on any history of a DSM-IV-TR axis I disorder before the behavioral task. For the current study, data of interest were available for 74 subjects (40 ANX/DEP and 34 HC youth). Table 1 describes lifetime diagnostic status and diagnostic status at the time of the most recent assessment in each group.
Table 1.
Demographic Characteristics by Diagnostic Group
| DEP/ANX (n = 40) | HC (n = 33) | p Value | |
|---|---|---|---|
| Age, years, M (SD) | 13.2 (1.0) | 12.6 (1.3) | 0.04* |
| Female, n (%) | 22 (55) | 22 (65) | 0.40 |
| Ethnicity, n (%) | |||
| White | 24 (60.0) | 17 (50.0) | 0.63 |
| Black | 14 (35.0) | 14 (41.2) | |
| Other | 2 (5.0) | 3 (8.8) | |
| IQ, M (SD) | 105.8 (14.3) | 109.1 (13.4) | 0.32 |
| SCARED, parent, M (SD) | 10.1 (6.6) | 6.9 (4.6) | 0.02* |
| SCARED, child, M (SD) | 13.8 (8.8) | 9.7 (6.3) | 0.04* |
| CDI, parent, M (SD) | 8.8 (5.5) | 6.8 (4.7) | 0.11 |
| CDI, child, M (SD) | 4.3 (3.7) | 2.5 (3.0) | 0.03* |
| Connors | |||
| Inattention | 3.2 (3.2) | 1.7 (1.8) | 0.02* |
| Hyperactivity | 2.8 (3.0) | 1.3 (1.7) | 0.01* |
| Executive Function | 4.1 (3.8) | 3.3 (3.0) | 0.30 |
| Most Recent Diagnostic Assessment: | |||
| Anxiety Disorder Only | 9 (22.5%) | 0 (0%) | |
| Depression Only | 0 (0%) | 0 (0%) | |
| Anxiety & Depression | 1 (2.5%) | 0 (0%) | |
| Neither Anxiety nor Depression | 30 (75%) | 0 (0%) | |
| Any History of: | |||
| Anxiety Disorder Only | 17 (42.5%) | 0 (0%) | |
| Depression Only | 8 (20%) | 0 (0%) | |
| Anxiety & Depression | 15 (37.5%) | 0 (0%) | |
| Neither Anxiety nor Depression | 0 (0%) | 0 (0%) | |
Note. The table presents demographic and clinical information for each group. Dep/Anx = depression and/or anxiety; HC = healthy controls; SCARED = Screen for Childhood Anxiety Related Emotional Disorders; CDI = Children's Depression Inventory.
= p < .05.
Tasks
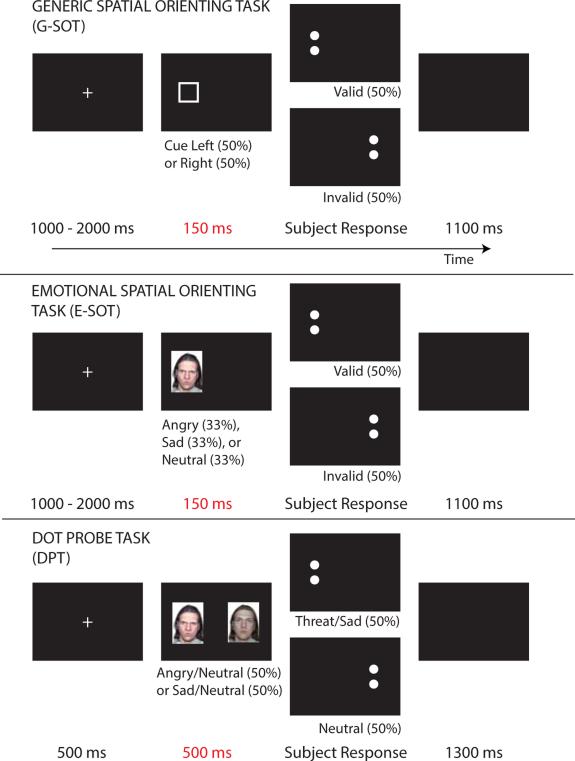
Testing was conducted in a darkened room with a trained research assistant and the child. Subjects were seated at a computer. In all tasks, subjects’ task was to discriminate whether a target pair of dots was oriented vertically (:) or horizontally (..) by pressing one of two buttons on a keyboard. Subjects were instructed to respond as quickly as possible without sacrificing accuracy. Accuracy was meant to be near ceiling and reaction time was the dependent measure. See Figure 1 for graphical depictions of each task.
Figure 1.
Attention tasks to measure stimulus-driven attention (G-SOT), threat bias and sad bias at 150ms (E-SOT), and threat bias and sad bias at 500ms (DPT). In each task, the trial begins with a central fixation cross followed by the presentation of a single box cue (G-SOT); a single face with a neutral, angry, sad expression (E-SOT); or a pair of faces with neutral and emotional expressions (DPT). Following the delay indicated in each panel in red, a target pair of dots appears randomly at the left or right location and the subjects’ task is to indicate with a button press whether the dots are oriented vertically or horizontally.
Generic Spatial Orienting Task (G-SOT): Subjects performed a standard spatial orienting task to measure stimulus-driven attention. A central fixation cross appeared for 500, 1000, or 1500ms (randomly) followed by the presentation of a square six degrees to the left or right of fixation. After 150ms, the square disappeared and the target pair of dots appeared randomly at the left or right position (no relationship between cue square and target). Following the subject making a button press response, a blank screen was presented for 1100ms before the next trial began. Stimulus-driven attention was calculated as the average reaction time to targets that appeared at the uncued location minus average reaction time to targets that appeared at the cued location. The higher the magnitude of stimulus-driven attention, therefore, the more strongly attention is captured by the square box cue.
Emotional Spatial Orienting Task (E-SOT): Procedures were identical to the generic stimulus-driven attention task except the cue was a single face with either an angry, sad, or neutral expression (selected randomly without replacement). Faces used in the E-SOT and the dot-probe task were a subset of the NimStim stimuli (Tottenham et al., 2009). Threat bias at 150ms was calculated as the average reaction time for targets at the same location as neutral cue faces minus reaction time for targets at the same location as angry cue faces. Note that angry faces cues and neutral face cues were presented on separate trials. Sad bias at 150ms was calculated in a parallel fashion using sad faces instead of angry faces. Because this measure of threat bias and sad bias depends only on reaction times to cued locations, this calculation represents increased engagement by emotional versus neutral faces (Koster et al., 2006). Threat bias measured with the E-SOT, therefore, indicates the degree to which angry faces more strongly capture attention compared to neutral faces.
Dot-Probe Task (DPT): Subjects performed a standard dot-probe task to measure threat bias and sad bias. Subjects viewed a central fixation cross for 500ms followed by the presentation of two faces (from the same actor), centered six degrees to the left and right of fixation. One of the two faces had a neutral expression while the other face had (randomly) either a sad or angry expression. Location of the neutral versus emotional face was selected at random. 500ms after stimulus onset, the faces disappeared and the target appeared randomly at the location of the neutral or emotional face. Following subject response, a blank screen was presented for 1300ms before the next trial began. Threat bias at 500ms was calculated as reaction time for targets that appeared at the location of neutral faces minus reaction time for targets that appeared at the location of angry faces in the subset of trials that had an angry face/neutral face stimulus pairing. Sad bias was calculated in a parallel fashion. Previous experimental work suggests that the measure of threat bias or sad bias as calculated by the dot probe represents both engagement with and difficulty with disengagement from the emotional stimuli (Klumpp & Amir, 2009; Koster, Crombez, Verschuere, & De Houwer, 2004). A higher value of threat bias measured with the DPT, therefore, could reflect either how strongly the angry face captures attention and/or how difficult it is for the subject to reorient to the location of the neutral face after the angry face has captured attention.
Experimental Procedure
Informed consent was obtained from parents and assent was obtained from all child participants. Parents completed questionnaires and rating scales while youth completed the experimental tasks. Subjects completed ten task blocks (two G-SOT, four E-SOT, and four DPT) each with 48 trials. Block order was selected at random with the stipulation that subjects had to complete one G-SOT block, two E-SOT blocks, and two DPT blocks before completing the remaining five blocks. During all task blocks, subjects placed their heads on a chin-rest in order to standardize the distance between head and screen for all subjects. Tasks were programmed in E-Prime (Psychology Software Tools, Pittsburgh, PA). Subjects were asked to redo task blocks in which performance accuracy was less than 80%.
During the same session, subjects and their parents completed parent and child versions of the Child Depression Inventory (CDI) and the Screen for Child Anxiety Related Disorders (SCARED) and the parent version of the Conners (to assess ADHD symptoms). Subjects and their parents also completed questionnaires regarding medication use in the past 48 hours. IQ was assessed at separate lab visits over the last four years using either the Wechsler Abbreviated Scale of Intelligence (WASI) or the Kaufman Brief Intelligence Test (K-BIT).
Data Analysis
Trials with incorrect responses and trials with reaction time greater than 3000ms were first removed. Next, for each task block type, trials with reaction time two standard deviations from the mean for that subject were removed. We also removed any subject average measure (e.g., threat bias with the DPT) that was two standard deviations from the sample mean.
To explore the spatial orienting tasks (G-SOT and E-SOT), we used a repeated measures ANCOVA with cue type (square box, angry face, sad face, neutral face) and cue location (valid: target appears at cued location versus invalid: target appears at uncued location) as within-subject factors. Age was included as a covariate because it was significantly related to stimulus-driven attention (see Results).
To test whether measures of stimulus driven attention, threat bias, and sad bias were significantly different from zero, we used one sample t-tests. We used a paired t-test to determine whether stimulus-driven attention measured using only the G-SOT was different from stimulus-driven attention using data from the G-SOT and the E-SOT. We used two sample t-tests to compare measures of threat bias, sad bias, and stimulus-driven attention in ANX/DEP versus HC. We additionally explored relationships between different tasks and clinical symptoms by computing Pearson's correlations. Correlations were compared to each other using Fisher's r-to-z transformation and comparing z-values with an online tool (Preacher, 2002). Where indicated in the results, age was included as a covariate in analyses.
RESULTS
Of the 97 individuals contacted for this study, 83 agreed to participate. Relative to subjects who participated, subjects who refused were more likely to be male, χ2 (1) = 4.7, p = .03, but there were no differences in diagnostic status, χ2 (1) = 1.7, p = .43; ethnicity, χ2 (2) = 0.03, p = .99; age, t(94) = 1.0, p = .30; or IQ, t(89) = 0.79, p = .43. One subject was excluded from all analyses because of excessively long reaction times across all tasks. Three of the children with a history of anxiety and/or depression (ANX/DEP) and three of the healthy controls (HC) had to redo task blocks because of accuracy less than 80%. Nine of the participants had a history of a psychiatric illness (e.g., ADHD) but no history of anxiety or depression; these subjects were excluded from analyses.
The following demographic data pertain to the 73 participating subjects with usable data and are summarized in Table 1. ANX/DEP participants were significantly older than HC, but there were no significant group differences in gender, ethnicity, or IQ. As expected, there were significant differences in a range of clinical symptoms between ANX/DEP and HC. Six ANX/DEP subjects reported psychotropic medication use in the past 24 hours (one on stimulant and antidepressant, one on stimulant and antipsychotic, three on antidepressant alone, and one on stimulant alone), compared to two HC subjects (both on stimulants alone). With one exception, detailed below, all significant results described below remained significant when the subjects using psychotropic medication in the past 24 hours were eliminated from analyses.
We assessed the relationship between task-based measures of attention and the following factors that were not the focus of the current study: sex, gender, and inattentive and hyperactivity symptoms based on parent report from the Connors. All relationships were non-significant with the exception of a significant negative correlation between age and stimulus-driven attention (r = −.27, p = .03). Based on this result, we controlled for age in all analyses described below that included stimulus-driven attention.
Attention biases and stimulus-driven attention
Means and standard deviations for all attention measures are listed in Table 1. The spatial orienting tasks (G-SOT and E-SOT) were explored with an ANCOVA examining the effects of cue type and cue location on reaction time. As expected, subjects had significantly faster reaction times at cued versus non-cued locations for all cue types (square box, angry face, sad face, neutral face) as indicated by a main effect of cue location, F(1,201) = 10.1, p = .002, partial η2 = .13. There was no main effect of cue type, F(3,201) = 0.53, p = .66, partial η2 = .008, nor was there an interaction between cue type and cue location, F(3,201) = 0.71, p = .55, partial η2 = .010, suggesting that all cue types manipulated stimulus-driven attention in an equivalent manner.
As expected on the basis of the omnibus ANCOVA described above, stimulus-driven attention, as measured by the G-SOT, was significantly greater than zero, M = 38.4ms, t(66) = 7.8, p < .001, d = 0.95. The omnibus ANCOVA suggests that there were no statistical differences between stimulus-driven orienting to the square box cues from the G-SOT and the three faces from the E-SOT. Nevertheless, in analyses below that examine relationships between stimulus-driven attention and attention biases, based on our original hypothesis, we use the measure of stimulus-driven attention derived only from the G-SOT. The pattern of results was unchanged when using data from both G-SOT and E-SOT as the measure of stimulus-driven attention.
The E-SOT was used to calculate attention bias for angry versus neutral faces (threat bias) as well as attention bias for sad versus neutral faces (sad bias) 150ms after the faces appeared. As expected on the basis of the null results from the omnibus ANCOVA described above, across all subjects there was no net threat bias, M = 2.4ms, t(67) = 0.39, p = .70, d = 0.05, nor sad bias, M = 3.4ms, t(68) = 0.63, p = .53, d = 0.08, at this shorter time interval. The dot probe task (DPT) was used to calculate threat bias and sad bias 500ms after the faces appeared. Averaged across all subjects, participants exhibited a significant bias towards threat, M = 11.1ms, t(66) = 2.5, p = .018, d = 0.30, but no bias towards or away from sad, M = −0.85ms, t(67) = 0.25, p = .80, d = 0.03, at this longer time interval.
To test the hypothesis that threat bias but not sad bias is associated with stimulus-driven attention, we examined the relationships between stimulus-driven attention, threat bias and sad bias at 150ms, and threat bias and sad bias at 500ms. Complete results are detailed in Table 3. Across all subjects, threat bias at 150ms was negatively correlated with threat bias at 500ms (r = −.26, p = .038), suggesting that early threat vigilance was associated with later threat avoidance. In addition, stimulus-driven attention was significantly negatively correlated with threat bias at 500ms across all subjects (r = −.28, p = .027), suggesting that rapid orientation to a generic, non-emotional cue is associated with threat avoidance at longer time intervals. Stimulus-driven attention was not, however, significantly correlated with threat bias at 150ms (r = −.024, p = .85). In contrast to threat bias, there were no significant correlations between sad bias at 500ms and either sad bias at 150ms (r = −.06, p = .62) or stimulus driven attention (r = −.11, p = .29). Across all subjects, threat bias and sad bias at 500ms were negatively correlated with each other (r = −.30, p = .017).
Table 3.
Correlations Among Measures of Attention by Diagnostic Group
| Stimulus-Driven Attn. | Threat Bias at 150ms | Threat Bias at 500ms | Sad Bias at 150ms | ||
|---|---|---|---|---|---|
| All Subjects (n = 73) | Threat Bias at 150ms | −0.04 | |||
| Threat Bias at 500ms | −0.28* | −0.26* | |||
| Sad Bias at 150ms | −0.12 | 0.14 | |||
| Sad Bias at 500ms | −0.09 | 0.20 | −0.29* | −0.02 | |
| History of Depression or Anxiety (n = 40) | Threat Bias at 150ms | 0.12 | |||
| Threat Bias at 500ms | −0.39* | −0.49** | |||
| Sad Bias at 150ms | 0.02 | −0.11 | |||
| Sad Bias at 500ms | −0.17 | 0.11 | −0.34* | −0.16 | |
| No History Depression or Anxiety (n = 33) | Threat Bias at 150ms | −0.25 | |||
| Threat Bias at 500ms | −0.17 | 0.00 | |||
| Sad Bias at 150ms | −0.27 | 0.33 | |||
| Sad Bias at 500ms | −0.03 | 0.35 | −0.12 | 0.21 | |
Note. Across-subject Pearson's correlations were computed between measures of stimulus-driven attention, threat bias, and sad bias in the entire sample (top row) and when the sample is divided into children with a history of anxiety and/or depression (middle row) and children with no psychiatric history (bottom row). No correlations are presented for threat bias at 150ms and sad bias at 150ms because both measures involve subtraction of average reaction time to valid neutral cues in the E-SOT, which could induce spurious correlations.
= p < .05
= p < .01.
Measures of attention and clinical symptoms
We examined whether the measures of attention described above varied depending on current symptoms or lifetime diagnosis of an anxiety disorder or depression. Correlations between current clinical symptoms and measures of attention are described in Table 4. Limited empirical data suggest that stimulus-driven attention may be positively correlated with current symptoms of anxiety but negatively correlated with current symptoms of depression. Consistent with these prior data, current depressive symptoms as measured by the CDI (averaged across parent and child reports) were significantly negatively correlated with stimulus-driven attention (r = −.26, p = .038; became non-significant when subjects using psychotropic medicines were removed). This correlation remained significant when using only parent report measures (r = −.32, p = .008, remained significant when subjects using psychotropic medications were removed) but not when using only child report (r = −.001, p = .99). Contrary to our expectations, we did not detect any relationship between stimulus-driven attention and current symptoms of anxiety as measured by the SCARED (r = −.02, p = .87). Furthermore, stimulus-driven attention was no different between youth with a prior history of a diagnosed anxiety disorder and/or depression (ANX/DEP) and healthy controls (HC), F(1,66) = 0.11, p = .74, partial η2 = .002.
Table 4.
Correlations Between Measures of Attention and Current Clinical Symptoms
| Anxiety Symptoms (based on SCARED) | Depression Symptoms (based on CDI) | |
|---|---|---|
| Stimulus-driven Attention | −0.03 | −0.26* |
| Threat Bias at 150ms | 0.17 | 0.12 |
| Threat Bias at 500ms | −0.15 | −0.01 |
| Sad Bias at 150ms | 0.23 | 0.07 |
| Sad Bias at 500ms | 0.22 | 0.30* |
Note. Across-subject Pearson's correlations were computed between measures of attention and current symptoms of anxiety and depression. Symptoms are averaged between and parent and child reporters.
= p < .05.
We next explored threat bias and sad bias in relation to current clinical symptoms and lifetime diagnostic history. Threat bias and sad bias at 150ms were not significantly related to current clinical symptoms, nor did these measures differ between ANX/DEP and HC (all p > 0.30). Current depressive symptoms, however, were significantly positively correlated with sad bias at 500ms (r = .30, p = .01). This correlation held when looking at child report alone (r = .24, p = .045) or parent report alone at trend level (r = .24, p = .053). Current symptoms of anxiety were not significantly correlated with threat bias at 500ms (r = −.15, p = .35). Concerning lifetime history of anxiety or depression, ANX/DEP exhibited neither a threat bias, M = 0.89ms, t(36) = 0.2, p = .87, d = 0.03, nor a sad bias, M = 6.6ms, t(37) = 1.6, p = .12, d = 0.26, at 500ms. These bias values were essentially unchanged when restricting threat bias calculations to the subset of ANX/DEP with a history of anxiety (0.13ms) and sad bias to those with a history of depression (1.8ms). HC, on the other hand, exhibited a significant attention bias towards threat at 500ms, M = 23.6ms threat bias, t(29) = 3.3, p = .003, d = 0.60, and a non-significant trend for an attention bias away from sad at 500ms, M = 10.2ms sad avoidance, t(29) = 2.0, p = .056, d = 0.37. Relative to HC children, ANX/DEP children had significantly lower attention bias towards threat versus neutral faces, M = 22.7ms difference, t(65) = 2.6, p = .012, d = 0.63, and significantly higher attention bias towards sad versus neutral faces, M = 16.9ms difference, t(66) = −2.6, p = .012, d = 0.63, at the interval 500ms following the onset of face pairs.
Prior history of an anxiety disorder or depression and the relationship between stimulus-driven attention and threat bias
Finally, we tested whether the significant relationships between stimulus-driven attention, threat bias at 150ms, and threat bias at 500ms, described above, varied depending on lifetime diagnostic history. We expected that all children, regardless of prior psychiatric history, would demonstrate a significant relationship between stimulus-driven attention and threat bias. Contrary to this prediction, the negative correlation between threat bias at 150ms and threat bias at 500ms was significant in the ANX/DEP group (r = −.41, p = .013) but not HC (r = .08, p = .69), and the ANX/DEP versus HC correlation values were significantly different from each other (p = .05; see methods for details). The negative correlation between stimulus-driven attention and threat bias at 500ms was significant in ANX/DEP (r = −.39, p = .023) but not HC (r = −.17, p = .38), although no difference was detected between groups. Figure 2 depicts these significant results for ANX/DEP graphically by illustrating that the 50% of subjects with the greatest threat avoidance at 500ms had greater threat vigilance at 150ms and greater measures of stimulus-driven attention relative to the other 50% of subjects. Finally, the negative correlation between threat bias at 500ms and sad bias at 500ms was significant in ANX/DEP (r = −.34, p = .04) but not HC (r = −.12, p = .55), but again this correlation was not significantly different between groups.
Figure 2.
Threat avoidance 500ms after the appearance of emotional faces is associated with threat vigilance at 150ms and increased stimulus-driven attention in youth with a history of an anxiety disorder and/or depression (ANX/DEP). Among ANX/DEP, attention bias to threat at 500ms is negatively correlated with both attention bias to threat at 150ms and stimulus-driven attention. To graphically depict these negative correlations, ANX/DEP subjects are divided in the 50% of subjects with the highest (red) and lowest (blue) threat bias at 500ms. (A) ANX/DEP Subjects with the lowest threat bias (or highest threat avoidance) at 500ms had the highest threat bias at 150ms. (B) ANX/DEP subjects with the lowest threat bias (or highest threat avoidance) at 500ms had the highest measures of stimulus-driven attention to a generic, non-emotional stimulus.
DISCUSSION
This study explored relationships between stimulus-driven attention, attention bias towards threatening stimuli, attention bias towards sad stimuli, and current clinical symptoms in school aged youth with a history of anxiety or depression as well as healthy controls. Results provide several pieces of evidence supporting the hypothesis that stimulus-driven attention is associated with threat bias but not sad bias in youth that have suffered from an anxiety disorder or depression. First, rapid vigilance to threatening stimuli was associated with later avoidance of threatening stimuli exclusively in children with a history of anxiety or depression. This vigilance-avoidance pattern of attention is consistent with stimulus-driven capture of attention by threatening stimuli. Second, rapid vigilance to generic, non-emotional cues (i.e., stimulus-driven attention) was likewise associated with later avoidance of threatening stimuli in children with a history of anxiety or depression. This result is consistent with the hypothesis that stimulus-driven attention is the mechanism underlying later avoidance of threat in children prone to anxiety or depression.
Attention bias towards threat is robustly associated with anxiety (Bar-Haim et al., 2007) and may be related to the etiology of anxiety disorders (Eldar et al., 2008; MacLeod et al., 2002). While altered attention to threat has been consistently reported in anxious youth, some studies report attention bias towards threat while others report attention bias away from threat (Pine et al., 2009; Puliafico & Kendall, 2006; Shechner et al., 2012). Persistent attention to threatening stimuli results in more time spent experiencing negative stimuli, conferring risk for anxiety and depression (Derryberry & Reed, 2002; Derryberry & Rothbart, 1997; Lonigan et al., 2004). In contrast, excessive behavioral avoidance may decrease the opportunity to learn that stimuli initially perceived as threatening are actually safe (Mowrer, 1960). While attention biases either towards or away from threat may therefore be problematic, the mechanisms underlying threat-related attention biases remain unclear.
The current results may explain why children with anxiety and depression, but not typically developing children, have a maladaptive pattern of attention to threatening stimuli. Results indicate that threatening stimuli appear to more effectively engage stimulus-driven attention in children prone to anxiety or depression. Stimulus-driven attention entails an involuntary, rapid (< 150ms) capture of attention by a salient stimulus followed by a shift of attention away from the location of the salient stimulus, referred to as inhibition of return (within 500ms) (Corbetta & Shulman, 2002; Klein, 2000). Results from the current study suggest that in children with a history of anxiety or depression, when threatening and non-threatening stimuli are presented simultaneously, the threatening stimulus captures stimulus-driven attention, resulting in an early vigilance followed by later avoidance of the threatening stimulus. This pattern is supported by the finding that the more vigilant the child was for threat initially (150ms), the more avoidant the child was at a later time point (500ms), consistent with the timing and pattern of stimulus-driven orienting. At least one other study has reported a similar correlation between early threat vigilance and later threat avoidance, albeit in children with no psychiatric history (Vervoort et al., 2011).
An additional finding in the current study supports the hypothesis that stimulus-driven attention is involved in attention bias towards threat. Among children with a history of anxiety or depression, the greater a child's magnitude of initial stimulus-driven orienting to generic, non-emotional cues, the more that child avoided threat at the later time interval. The most succinct explanation of this result is that children with faster initial stimulus-driven orienting also have faster inhibition of return. Since inhibition of return may be driving threat avoidance at later time intervals, greater inhibition of return results in greater threat avoidance. These findings suggest that stimulus-driven orienting may underlie threat vigilance and threat avoidance in children with a history of anxiety or depression.
Critically, the link between early threat vigilance and later threat avoidance was present only in children with a history of anxiety or depression and not in children without a psychiatric history. This pattern of results suggests that threatening stimuli are more likely to capture stimulus-driven attention in children with a history of anxiety or depression. Individual differences in the speed of stimulus-driven orienting, therefore, may only relate to individual differences in attention to threat in children with a history of anxiety or depression.
It is important to note that our measure of early threat bias reflects faster engagement of attention by angry versus neutral faces (Koster et al., 2006) while the measures of both generic stimulus-driven attention and late threat bias reflect a mixture of engagement by and disengagement from generic and emotional cues (see methods for details) (Klumpp & Amir, 2009; Koster et al., 2004). Although the complex nature of these tasks complicates interpretation, the most succinct explanation is that subjects with fast engagement of threat at 150ms were the fastest to disengage the threatening stimulus and attend to the neutral stimulus at 500ms. The alternative explanation is that subjects with fast engagement of threat 150ms after the stimulus appeared had slow engagement of threat 500ms after stimuli appeared, which is highly counterintuitive. Nevertheless, we completely cannot rule out task differences as an explanation for the negative correlation between threat bias at 150ms and threat bias at 500ms.
The most straightforward explanation of our results is that the initial rapid orienting phase of stimulus-driven attention is associated with early threat vigilance, and the later inhibition of return phase is associated with threat avoidance. Alternatively, previous investigators have suggested that the later avoidance of threatening stimuli in anxious children is a voluntary, adaptive process that serves to minimize distress. Consistent with this hypothesis, previous work suggests that while all children appear to attend to threat at early time intervals, children with greater effortful control are more likely to avoid threatening stimuli at longer time intervals (Derryberry & Reed, 2002; Lonigan & Vasey, 2009; Lonigan et al., 2004). Another explanation that reconciles this previous work with current results is that children with more rapid early vigilance to threat more strongly voluntarily avoid threat at later time intervals.
As stated above, the literature in pediatric samples is mixed, with studies reporting both threat vigilance and threat avoidance associated with anxiety. In the current study, children with no psychiatric history exhibited an attention bias towards threat and an attention bias away from sad stimuli relative to children with a history of anxiety or depression. Many factors likely contribute to the variation across studies including subject age, degree of perceived threat during the experiment, duration of stimulus presentation, and the specific anxiety disorders studied (Shechner et al., 2012). The current study lends support to the vigilance-avoidance pattern of attention to threat (Cisler & Koster, 2010; Mogg et al., 2004) indicating that attention bias towards versus away from threat may depend on the duration of stimulus presentation. It is also important to consider that most of the children in the clinical group no longer met criteria for an anxiety disorder or depression at the time of the study, and so results may be related to a trait characteristic or a marker of recovery rather than ongoing symptoms.
An understanding of the mechanisms and timing underlying attention biases in children with anxiety and depression is important because computer-based tasks have been shown to reverse attention biases and improve symptoms (Eldar et al., 2012; Lowther & Newman, 2014). While attention bias modification shows promise as an emerging treatment, effect sizes are relatively small and benefits are inconsistent (Mogoase, David, & Koster, 2014). Most forms of attention bias modification rely on a variation of the dot-probe task with angry and neutral faces presented for 500ms, although at least one prior study in youth has tested a modification of the spatial orienting paradigm (Bar-Haim, Morag, & Glickman, 2011). The current study suggests that attention bias modification programs aimed at altering threat bias should focus on altering stimulus-driven attention to threatening stimuli. Attention bias modification paradigms should test using shorter stimulus presentation durations (e.g., 150ms) that would more directly engage stimulus-driven attention. Further work is needed to understand the mechanisms underlying attention biases to inform attention bias modification designs.
In addition to attention biases towards negative stimuli, theoretical work suggests that there are alterations in basic attention mechanisms in anxiety and depression irrespective of the emotional content of stimuli. According to Eysenck's attentional control theory, anxiety disorders are associated with increased stimulus-driven attention and decreased goal-directed attention (Eysenck et al., 2007). As a result, individuals with anxiety disorders are more likely to attend to novel stimuli, which are often interpreted as threatening. Depression, on the other hand, has been associated with a range of cognitive deficits (Gotlib & Joormann, 2010), and may include deficits in both goal-directed and stimulus-driven attention. As with attention biases, any changes in basic attention mechanisms in youth with anxiety or depression would be highly relevant to understanding the pathophysiology and the design of treatments – such as training stimulus-driven or goal-directed attention directly. In the current study, consistent with overall cognitive deficits in depression, increasing symptoms of current depression were associated with lower measures of stimulus-driven attention. We did not detect a relationship between current anxiety symptoms and stimulus-driven attention. Given that our sample included mostly individuals who had recovered from depression and anxiety, more work is needed in actively anxious or depressed samples.
It is important to consider the current results in light of several limitations. We compared typically developing children to children with a history of depression and/or an anxiety disorder, most of whom no longer met criteria for either disorder at their most recent assessment. It is unclear whether results from actively ill youth would differ. In addition, because of high rates of co-morbidity in the study sample, we did not have sufficient power to separately analyze youth with a history of depression only versus youth with a history of anxiety disorders only. Finally, the study was limited by a relatively small sample size and narrow age range.
This study provides several pieces of evidence supporting the hypothesis that stimulus-driven attention is associated with threat bias but not sad bias in youth that have suffered from an anxiety disorder or depression. Current estimates suggest that around 30% of youth experience an anxiety disorder or depression (Merikangas et al., 2010), and most adults with anxiety or depression experienced symptoms during childhood or adolescence (Kessler et al., 2005). Given the impairing nature of these illnesses and the evidence that attention biases may have an etiological relationship to these disorders, studies such as the current investigation that explore associations between basic attention processes and negative attention biases are needed to better understand the developmental pathophysiology and inform treatment development.
Table 2.
Measures of Attention by Diagnostic Group
| Stimulus-Driven Attn. | Threat Bias at 150ms | Threat Bias at 500ms | Sad Bias at 150ms | Sad Bias at 500ms | |
|---|---|---|---|---|---|
| All Subjects | 38.4 (40.4) | 2.4 (51.1) | 11.1 (37.2) | 3.4 (44.5) | −0.9 (27.9) |
| History of Dep/Anx | 37.5 (39.2) | 3.1 (55.1) | 0.9 (39.2) | −0.18 (46.6) | 6.6 (25.4) |
| No History of Dep/Anx | 39.5 (42.3) | 1.7 (46.8) | 23.6 (39.4) | 1.7 (46.8) | −10.2 (28.3) |
Note. This table presents means and standard deviations (in parentheses) in milliseconds for the measures of attention for the entire sample (top row), for children with a history of anxiety and/or depression (middle row) and children with no psychiatric history (bottom row). Dep/Anx = depression and/or anxiety; Attn = attention.
REFERENCES
- Amir N, Elias J, Klumpp H, Przeworski A. Attentional bias to threat in social phobia: Facilitated processing of threat or difficulty disengaging attention from threat? Behaviour Research and Therapy. 2003;41:1325–1335. doi: 10.1016/s0005-7967(03)00039-1. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA). Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. doi: 10.1097/00004583-200001000-00015. doi: 10.1097/00004583-200001000-00015. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van IJzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Morag I, Glickman S. Training anxious children to disengage attention from threat: A randomized controlled trial. Journal of Child Psychology and Psychiatry. 2011;52:861–869. doi: 10.1111/j.1469-7610.2011.02368.x. doi: 10.1111/j.1469-7610.2011.02368.x. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Bradley BP, Mogg K, Lee SC. Attentional biases for negative information in induced and naturally occurring dysphoria. Behaviour Research and Therapy. 1997;35:911–927. doi: 10.1016/s0005-7967(97)00053-3. [DOI] [PubMed] [Google Scholar]
- Britton JC, Bar-Haim Y, Carver FW, Holroyd T, Norcross MA, Detloff A, Pine DS. Isolating neural components of threat bias in pediatric anxiety. Journal of Child Psychology and Psychiatry. 2012;53:678–686. doi: 10.1111/j.1469-7610.2011.02503.x. doi: 10.1111/j.1469-7610.2011.02503.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown HM, McAdams TA, Lester KJ, Goodman R, Clark DM, Eley TC. Attentional threat avoidance and familial risk are independently associated with childhood anxiety disorders. Journal of Child Psychology and Psychiatry. 2013;54:678–685. doi: 10.1111/jcpp.12024. doi: 10.1111/jcpp.12024. [DOI] [PubMed] [Google Scholar]
- Browning M, Holmes EA, Charles M, Cowen PJ, Harmer CJ. Using attentional bias modification as a cognitive vaccine against depression. Biological Psychiatry. 2012;72:572–579. doi: 10.1016/j.biopsych.2012.04.014. doi: 10.1016/j.biopsych.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruder GE, Kayser J, Tenke CE, Leite P, Schneier FR, Stewart JW, Quitkin FM. Cognitive ERPs in depressive and anxiety disorders during tonal and phonetic oddball tasks. Clinical Electroencephalography. 2002;33:119–124. doi: 10.1177/155005940203300308. [DOI] [PubMed] [Google Scholar]
- Chica AB, Bartolomeo P, Lupianez J. Two cognitive and neural systems for endogenous and exogenous spatial attention. Behavioural Brain Research. 2013;237:107–123. doi: 10.1016/j.bbr.2012.09.027. doi: 10.1016/j.bbr.2012.09.027. [DOI] [PubMed] [Google Scholar]
- Cisler JM, Koster EH. Mechanisms of attentional biases towards threat in anxiety disorders: An integrative review. Clinical Psychology Review. 2010;30:203–216. doi: 10.1016/j.cpr.2009.11.003. doi: 10.1016/j.cpr.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbetta M, Shulman GL. Control of goal-directed and stimulus-driven attention in the brain. Nature Reviews Neuroscience. 2002;3:201–215. doi: 10.1038/nrn755. doi: 10.1038/nrn755. [DOI] [PubMed] [Google Scholar]
- Dalgleish T, Taghavi R, Neshat-Doost H, Moradi A, Canterbury R, Yule W. Patterns of processing bias for emotional information across clinical disorders: A comparison of attention, memory, and prospective cognition in children and adolescents with depression, generalized anxiety, and posttraumatic stress disorder. Journal of Clinical Child and Adolescent Psychology. 2003;32:10–21. doi: 10.1207/S15374424JCCP3201_02. doi: 10.1207/S15374424JCCP3201_02. [DOI] [PubMed] [Google Scholar]
- Derryberry D, Reed MA. Anxiety-related attentional biases and their regulation by attentional control. Journal of Abnormal Psychology. 2002;111:225–236. doi: 10.1037//0021-843x.111.2.225. [DOI] [PubMed] [Google Scholar]
- Derryberry D, Rothbart MK. Reactive and effortful processes in the organization of temperament. Development and Psychopathology. 1997;9:633–652. doi: 10.1017/s0954579497001375. [DOI] [PubMed] [Google Scholar]
- Egger HL, Ascher B, Angold A. The preschool age psychiatric assessment: Version 1.4. Duke University Medical Center; Durham, NC: 2003. [Google Scholar]
- Eldar S, Apter A, Lotan D, Edgar KP, Naim R, Fox NA, Bar-Haim Y. Attention bias modification treatment for pediatric anxiety disorders: a randomized controlled trial. The American Journal of Psychiatry. 2012;169:213–220. doi: 10.1176/appi.ajp.2011.11060886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldar S, Ricon T, Bar-Haim Y. Plasticity in attention: Implications for stress response in children. Behaviour Research and Therapy. 2008;46:450–461. doi: 10.1016/j.brat.2008.01.012. doi: 10.1016/j.brat.2008.01.012. [DOI] [PubMed] [Google Scholar]
- Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: Attentional control theory. Emotion. 2007;7:336–353. doi: 10.1037/1528-3542.7.2.336. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- Fox E, Russo R, Bowles R, Dutton K. Do threatening stimuli draw or hold visual attention in subclinical anxiety? Journal of Experimental Psychology: General. 2001;130:681–700. [PMC free article] [PubMed] [Google Scholar]
- Fox NA, Henderson HA, Marshall PJ, Nichols KE, Ghera MM. Behavioral inhibition: Linking biology and behavior within a developmental framework. Annual Review of Psychology. 2005;56:235–262. doi: 10.1146/annurev.psych.55.090902.141532. doi: 10.1146/annurev.psych.55.090902.141532. [DOI] [PubMed] [Google Scholar]
- Gaffrey MS, Belden AC, Luby JL. The 2-week duration criterion and severity and course of early childhood depression: Implications for nosology. Journal of Affective Disorders. 2011;133:537–545. doi: 10.1016/j.jad.2011.04.056. doi: 10.1016/j.jad.2011.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb BE, Benas JS, Grassia M, McGeary J. Children's attentional biases and 5-HTTLPR genotype: Potential mechanisms linking mother and child depression. Journal of Clinical Child and Adolescent Psychology. 2009;38:415–426. doi: 10.1080/15374410902851705. doi: 10.1080/15374410902851705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib IH, Joormann J. Cognition and depression: Current status and future directions. Annual Review of Clinical Psychology. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, Pine DS. Attention bias modification treatment: A meta-analysis toward the establishment of novel treatment for anxiety. Biological Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Gibb BE, Abela JRZ, Flory K. Selective attention to affective stimuli and clinical depression among youths: Role of anxiety and specificity of emotion. Journal of Abnormal Psychology. 2010;119:491–501. doi: 10.1037/a0019609. doi: 10.1037/a0019609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison AJ, Gibb BE. Attentional biases in currently depressed children: An eye-tracking study of biases in sustained attention to emotional stimuli. Journal of Clinical Child and Adolescent Psychology. 2014:1–7. doi: 10.1080/15374416.2014.930688. doi: 10.1080/15374416.2014.930688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan AM, Butterfield EL, Phillips L, Hadwin JA. Brain response to unexpected novel noises in children with low and high trait anxiety. Journal of Cognitive Neuroscience. 2007;19:25–31. doi: 10.1162/jocn.2007.19.1.25. doi: 10.1162/jocn.2007.19.1.25. [DOI] [PubMed] [Google Scholar]
- In-Albon T, Kossowsky J, Schneider S. Vigilance and avoidance of threat in the eye movements of children with separation anxiety disorder. Journal of Abnormal Child Psychology. 2010;38:225–235. doi: 10.1007/s10802-009-9359-4. doi: 10.1007/s10802-009-9359-4. [DOI] [PubMed] [Google Scholar]
- Joormann J, Talbot L, Gotlib IH. Biased processing of emotional information in girls at risk for depression. Journal of Abnormal Psychology. 2007;116:135–143. doi: 10.1037/0021-843X.116.1.135. doi: 10.1037/0021-843X.116.1.135. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Klein R. Inhibition of return. Trends in Cognitive Sciences. 2000;4:138–147. doi: 10.1016/s1364-6613(00)01452-2. [DOI] [PubMed] [Google Scholar]
- Klumpp H, Amir N. Examination of vigilance and disengagement of threat in social anxiety with a probe detection task. Anxiety Stress and Coping. 2009;22:283–296. doi: 10.1080/10615800802449602. doi: 10.1080/10615800802449602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koster EH, Baert S, Bockstaele M, De Raedt R. Attentional retraining procedures: manipulating early or late components of attentional bias? Emotion. 2010;10:230–236. doi: 10.1037/a0018424. doi: 10.1037/a0018424. [DOI] [PubMed] [Google Scholar]
- Koster EH, Crombez G, Verschuere B, De Houwer J. Selective attention to threat in the dot probe paradigm: Differentiating vigilance and difficulty to disengage. Behaviour Research and Therapy. 2004;42:1183–1192. doi: 10.1016/j.brat.2003.08.001. doi: 10.1016/j.brat.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Koster EH, Crombez G, Verschuere B, Van Damme S, Wiersema JR. Components of attentional bias to threat in high trait anxiety: Facilitated engagement, impaired disengagement, and attentional avoidance. Behaviour Research and Therapy. 2006;44:1757–1771. doi: 10.1016/j.brat.2005.12.011. doi: 10.1016/j.brat.2005.12.011. [DOI] [PubMed] [Google Scholar]
- Koster EH, Verschuere B, Crombez G, Van Damme S. Time-course of attention for threatening pictures in high and low trait anxiety. Behaviour Research and Therapy. 2005;43:1087–1098. doi: 10.1016/j.brat.2004.08.004. doi: 10.1016/j.brat.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Kujawa AJ, Torpey D, Kim J, Hajcak G, Rose S, Gotlib IH, Klein DN. Attentional biases for emotional faces in young children of mothers with chronic or recurrent depression. Journal of Abnormal Child Psychology. 2011;39:125–135. doi: 10.1007/s10802-010-9438-6. doi: 10.1007/s10802-010-9438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Hu Y, Liu T, Wu D. Dipole source analysis of auditory P300 response in depressive and anxiety disorders. Cognitive Neurodynamics. 2011;5:221–229. doi: 10.1007/s11571-011-9156-y. doi: 10.1007/s11571-011-9156-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonigan CJ, Vasey MW. Negative affectivity, effortful control, and attention to threat-relevant stimuli. Journal of Abnormal Child Psychology. 2009;37:387–399. doi: 10.1007/s10802-008-9284-y. doi: 10.1007/s10802-008-9284-y. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Vasey MW, Phillips BM, Hazen RA. Temperament, anxiety, and the processing of threat-relevant stimuli. Journal of Clinical Child and Adolescent Psychology. 2004;33:8–20. doi: 10.1207/S15374424JCCP3301_2. doi: 10.1207/S15374424JCCP3301_2. [DOI] [PubMed] [Google Scholar]
- Lowther H, Newman E. Attention bias modification (ABM) as a treatment for child and adolescent anxiety: A systematic review. Journal of Affective Disorders. 2014;168:125–135. doi: 10.1016/j.jad.2014.06.051. doi: 10.1016/j.jad.2014.06.051. [DOI] [PubMed] [Google Scholar]
- Luby JL, Belden AC, Pautsch J, Si X, Spitznagel E. The clinical significance of preschool depression: Impairment in functioning and clinical markers of the disorder. Journal of Affective Disorders. 2009;112:111–119. doi: 10.1016/j.jad.2008.03.026. doi: 10.1016/j.jad.2008.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: Homotypic continuity and course over 24 months. Archives of General Psychiatry. 2009;66:897–905. doi: 10.1001/archgenpsychiatry.2009.97. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- lv J, Zhao L, Gong J, Chen C, Miao D. Event-related potential based evidence of cognitive dysfunction in patients during the first episode of depression using a novelty oddball task. Psychiatry Research. 2010;182:58–66. doi: 10.1016/j.pscychresns.2010.02.005. doi: 10.1016/j.pscychresns.2010.02.005. [DOI] [PubMed] [Google Scholar]
- MacLeod C, Rutherford E, Campbell L, Ebsworthy G, Holker L. Selective attention and emotional vulnerability: Assessing the causal basis of their association through the experimental manipulation of attentional bias. Journal of Abnormal Psychology. 2002;111:107–123. [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogg K, Bradley BP, de Bono J, Painter M. Time course of attentional bias for threat information in non-clinical anxiety. Behaviour Research and Therapy. 1997;35:297–303. doi: 10.1016/s0005-7967(96)00109-x. [DOI] [PubMed] [Google Scholar]
- Mogg K, Bradley BP, Miles F, Dixon R. Time course of attentional bias for threat scenes: Testing the vigilance-avoidance hypothesis. Cognition & Emotion. 2004;18:689–700. [Google Scholar]
- Mogg K, Wilson KA, Hayward C, Cunning D, Bradley BP. Attentional biases for threat in at-risk daughters and mothers with lifetime panic disorder. Journal of Abnormal Psychology. 2012;121:852–862. doi: 10.1037/a0028052. doi: 10.1037/a0028052. [DOI] [PubMed] [Google Scholar]
- Mogoase C, David D, Koster EH. Clinical efficacy of attentional bias modification procedures: An updated meta-analysis. Journal of Clinical Psychology. 2014 doi: 10.1002/jclp.22081. doi: 10.1002/jclp.22081. [DOI] [PubMed] [Google Scholar]
- Monk CS, Nelson EE, McClure EB, Mogg K, Bradley BP, Leibenluft E, Pine DS. Ventrolateral prefrontal cortex activation and attentional bias in response to angry faces in adolescents with generalized anxiety disorder. The American Journal of Psychiatry. 2006;163:1091–1097. doi: 10.1176/ajp.2006.163.6.1091. doi: 10.1176/appi.ajp.163.6.1091. [DOI] [PubMed] [Google Scholar]
- Mowrer OH. Learning Theory and Behavior. John Wiley & Sons; New York, NY: 1960. [Google Scholar]
- Pacheco-Unguetti AP, Acosta A, Callejas A, Lupiáñez J. Attention and anxiety: Different attentional functioning under state and trait anxiety. Psychological Science. 2010;21:298–304. doi: 10.1177/0956797609359624. doi: 10.1177/0956797609359624. [DOI] [PubMed] [Google Scholar]
- Peckham AD, McHugh RK, Otto MW. A meta-analysis of the magnitude of biased attention in depression. Depression and Anxiety. 2010;27:1135–1142. doi: 10.1002/da.20755. doi: 10.1002/da.20755. [DOI] [PubMed] [Google Scholar]
- Pérez-Edgar K, Bar-Haim Y, McDermott JM, Chronis-Tuscano A, Pine DS, Fox NA. Attention biases to threat and behavioral inhibition in early childhood shape adolescent social withdrawal. Emotion. 2010;10:349–357. doi: 10.1037/a0018486. doi: 10.1037/a0018486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Edgar K, Reeb-Sutherland BC, McDermott JM, White LK, Henderson HA, Degnan KA, Fox NA. Attention biases to threat link behavioral inhibition to social withdrawal over time in very young children. Journal of Abnormal Child Psychology. 2011;39:885–895. doi: 10.1007/s10802-011-9495-5. doi: 10.1007/s10802-011-9495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS. Research review: A neuroscience framework for pediatric anxiety disorders. Journal of Child Psychology and Psychiatry. 2007;48:631–648. doi: 10.1111/j.1469-7610.2007.01751.x. doi: 10.1111/j.1469-7610.2007.01751.x. [DOI] [PubMed] [Google Scholar]
- Pine DS, Helfinstein SM, Bar-Haim Y, Nelson E, Fox NA. Challenges in developing novel treatments for childhood disorders: Lessons from research on anxiety. Neuropsychopharmacology. 2009;34:213–228. doi: 10.1038/npp.2008.113. doi: 10.1038/npp.2008.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ. [August 7, 2014];Calculation for the test of the difference between two independent correlation coefficients. 2002 http://quantpsy.org. Retrieved from http://quantpsy.org.
- Puliafico AC, Kendall PC. Threat-related attentional bias in anxious youth: a review. Clinical Child and Family Psychology Review. 2006;9:162–180. doi: 10.1007/s10567-006-0009-x. doi: 10.1007/s10567-006-0009-x. [DOI] [PubMed] [Google Scholar]
- Roy AK, Vasa RA, Bruck M, Mogg K, Bradley BP, Sweeney M, Team C. Attention bias toward threat in pediatric anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:1189–1196. doi: 10.1097/CHI.0b013e3181825ace. doi: 10.1097/CHI.0b013e3181825ace. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez A, Vazquez C, Marker C, LeMoult J, Joormann J. Attentional disengagement predicts stress recovery in depression: An eye-tracking study. Journal of Abnormal Psychology. 2013;122:303–313. doi: 10.1037/a0031529. doi: 10.1037/a0031529. [DOI] [PubMed] [Google Scholar]
- Seefeldt WL, Kramer M, Tuschen-Caffier B, Heinrichs N. Hypervigilance and avoidance in visual attention in children with social phobia. Journal of Behavior Therapy and Experimental Psychiatry. 2014;45:105–112. doi: 10.1016/j.jbtep.2013.09.004. doi: 10.1016/j.jbtep.2013.09.004. [DOI] [PubMed] [Google Scholar]
- Shechner T, Britton JC, Pérez-Edgar K, Bar-Haim Y, Ernst M, Fox NA, Pine DS. Attention biases, anxiety, and development: Toward or away from threats or rewards? Depression and Anxiety. 2012;29:282–294. doi: 10.1002/da.20914. doi: 10.1002/da.20914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechner T, Jarcho JM, Britton JC, Leibenluft E, Pine DS, Nelson EE. Attention bias of anxious youth during extended exposure of emotional face pairs: A eye-tracking study. Depression and Anxiety. 2013;30:14–21. doi: 10.1002/da.21986. doi: 10.1002/da.21986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechner T, Rimon-Chakir A, Britton JC, Lotan D, Apter A, Bliese PD, Bar-Haim Y. Attention bias modification treatment augmenting effects on cognitive behavioral therapy in children with anxiety: randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53:61–71. doi: 10.1016/j.jaac.2013.09.016. doi: 10.1016/j.jaac.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvester CM, Barch DM, Corbetta M, Power JD, Schlaggar BL, Luby JL. Resting state functional connectivity of the ventral attention network in children with a history of depression or anxiety. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:1326–1336. e1325. doi: 10.1016/j.jaac.2013.10.001. doi: 10.1016/j.jaac.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvester CM, Corbetta M, Raichle ME, Rodebaugh TL, Schlaggar BL, Sheline YI, Lenze EJ. Functional network dysfunction in anxiety and anxiety disorders. Trends in Neurosciences. 2012;35:527–535. doi: 10.1016/j.tins.2012.04.012. doi: 10.1016/j.tins.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taghavi MR, Neshat-Doost HT, Moradi AR, Yule W, Dalgleish T. Biases in visual attention in children and adolescents with clinical anxiety and mixed anxiety-depression. Journal of Abnormal Child Psychology. 1999;27:215–223. doi: 10.1023/a:1021952407074. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Joormann J, Steinman SA, Gotlib IH. Automaticity in anxiety disorders and major depressive disorder. Clinical Psychology Review. 2012;32:575–603. doi: 10.1016/j.cpr.2012.06.004. doi: 10.1016/j.cpr.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry T, Nurse M, Hare TA, Nelson C. The NimStim set of facial expressions: Judgments from untrained research participants. Psychiatry Research. 2009;168:242–249. doi: 10.1016/j.psychres.2008.05.006. doi: 10.1016/j.psychres.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasey MW, Daleiden EL, Williams LL, Brown LM. Biased attention in childhood anxiety disorders: A preliminary study. Journal of Abnormal Child Psychology. 1995;23:267–279. doi: 10.1007/BF01447092. [DOI] [PubMed] [Google Scholar]
- Vervoort L, Wolters LH, Hogendoorn SM, Prins PJ, de Haan E, Boer F, Hartman CA. Temperament, attentional processes, and anxiety: Diverging links between adolescents with and without anxiety disorders? Journal of Clinical Child and Adolescent Psychology. 2011;40:144–155. doi: 10.1080/15374416.2011.533412. doi: 10.1080/15374416.2011.533412. [DOI] [PubMed] [Google Scholar]
- Waters AM, Henry J, Mogg K, Bradley BP, Pine DS. Attentional bias towards angry faces in childhood anxiety disorders. Journal of Behavior Therapy and Experimental Psychiatry. 2010;41:158–164. doi: 10.1016/j.jbtep.2009.12.001. doi: 10.1016/j.jbtep.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Waters AM, Mogg K, Bradley BP, Pine DS. Attentional bias for emotional faces in children with generalized anxiety disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:435–442. doi: 10.1097/CHI.0b013e3181642992. doi: 10.1097/CHI.0b013e3181642992. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Watts FN, MacLeod C, Mathews A. Cognitive Psychology and Emotional Disorders. 2nd ed. Wiley; Chichester: 1997. [Google Scholar]